Click on the boxes to see answers to common questions about colonoscopy procedures.
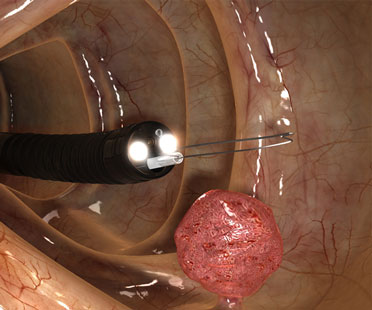
Colonoscopy is a procedure which enables the direct visualization of the lining of your colon (large intestine). A thin, flexible tube called a colonoscope, which has its own lens and light source, is inserted into the anus and slowly advanced from the rectum to the cecum (the anatomic beginning of the colon). Lesions such as polyps and colon cancer, and inflammation can be found during a colonoscopy. Biopsies can be obtained, and most polyps can be removed during a colonoscopy.
The preparation involves going on a clear liquid diet for 24 hours prior to the procedure. In addition, a laxative preparation is taken the night before and again, approximately 5 hours, prior to the procedure. Recent research has shown that “split dosing” leads to a better visualization of the colon. The colon must be completely clean for the procedure to be accurate and complete, so it is important to follow the instructions carefully. More specific instructions will be given to you when you schedule a colonoscopy. Please refer to our Precedure Instructions section in our website for more details.
Most medications can be continued as usual, but some medications can interfere with the preparation or the examination. Inform us about medications you’re taking, particularly aspirin products, arthritis medications, anticoagulants (blood thinners), insulin or iron products. Aspirin is usually held for 7 days.
Alert us if you require antibiotics prior to dental procedures, because you might need antibiotics before a colonoscopy as well.
Colonoscopy is well-tolerated and pain-free. You will be given a sedative by our anesthesiologist who will be present to monitor your vital signs during the examination.
You will lie on your side or back during the procedure. The procedure itself usually lasts approximately 20 minutes, although you should plan on one to two hours for waiting, preparation and recovery.
In some cases, the colonoscopy may not be completed due to a variation in the person’s colon anatomy and concern for a higher risk of a perforation. In this case, we may recommend a CT colonography (“virtual colonoscopy”) or a barium enema to visualize the portions of the colon which were not visualized during the colonoscopy.
If an area needs further evaluation, a biopsy may be obtained. If polyps are found during colonoscopy, they will most likely be removed during the examination.
Polyps are abnormal growths in the colon lining that are usually benign (noncancerous). They vary in size from a tiny dot to several inches. Because cancer begins in polyps, removing them is an important means of preventing colorectal cancer.
Tiny polyps may be destroyed by fulguration (burning) or by removing them with wire loops called snares or with biopsy instruments. A technique called “snare polypectomy” is used to remove larger polyps. This technique involves passing a wire loop through the colonoscope and removing the polyp from the intestinal wall using an electrical current. You should feel no pain during the polypectomy.
The results of the examination will be discussed with you. If a biopsy was taken or a polyp was removed, the material is sent to a pathology lab and the results are available in approximately 5 business days. You will be contacted by phone by one of our nurses.
You will not be allowed to drive for 12 hours. You will need to arrange for someone to escort you home from our office. Even if you feel alert after the procedure, your judgment and reflexes could be impaired for the rest of the day. You might have some cramping or bloating because of air that is introduced into the colon during the examination. This should disappear quickly when you pass gas.
You should be able to eat after the examination.
Complications are uncommon but may include a perforation, or tear, through the bowel wall that could require surgery. Bleeding might occur at the site of biopsy or polypectomy, but it’s usually minor. Bleeding can stop on its own or be controlled through the colonoscope; it rarely requires follow-up treatment. Some patients might have a reaction to the sedative agent.
Although complications after colonoscopy are uncommon, it’s important to recognize early signs of possible complications. Contact us immediately if you notice severe abdominal pain, fever and chills, or rectal bleeding of more than one-half cup. Note that bleeding can occur several days after the procedure.